Dehydration is more than just a lack of water; it can significantly impact your health, including your blood pressure. When your body is dehydrated, it compensates by constricting blood vessels, which can lead to elevated blood pressure levels. This connection is particularly crucial for individuals managing hypertension or those at risk. Understanding how dehydration affects your cardiovascular health is essential for making informed choices about hydration, especially during hot weather or after intense physical activity.
As you read on, you’ll discover the science behind dehydration and blood pressure, insights into monitoring your hydration status, and practical tips for maintaining optimal health. Empower yourself with knowledge that could help control your blood pressure and enhance your overall well-being. Your health is in your hands-let’s explore the vital relationship between hydration and heart health together.
Does Dehydration Impact Blood Pressure Levels?
Dehydration can significantly impact blood pressure levels, creating a complex relationship that can affect overall cardiovascular health. When the body loses more fluids than it takes in, it can lead to a decrease in blood volume. This reduced blood volume forces the heart to work harder to maintain adequate blood flow and pressure, potentially resulting in an elevation of blood pressure. This is particularly significant in individuals who already experience hypertension or other cardiovascular conditions, as dehydration can exacerbate their health issues.
To further understand the connection, consider the physiological role of fluids in the body. Hydration is crucial for maintaining the viscosity of the blood, which allows it to flow properly through the blood vessels. When dehydrated, blood becomes thicker, increasing the resistance the heart must overcome during circulation. Consequently, this can lead to higher systolic and diastolic pressures, leading to a heightened risk of cardiovascular events like strokes or heart attacks.
Additionally, dehydration can influence the body’s regulatory systems. The renin-angiotensin-aldosterone system (RAAS) plays a critical role in managing blood pressure and fluid balance. When dehydration occurs, the RAAS is activated, triggering the release of hormones that constrict blood vessels and raise blood pressure to conserve water and maintain organ perfusion. Over time, this persistent elevation in blood pressure due to chronic dehydration can contribute to sustained hypertension, further increasing risks for heart and kidney diseases.
To mitigate these risks, it’s essential to maintain optimal hydration levels. Drinking adequate amounts of water daily, especially during hot weather or exercise, is vital. Individuals should also monitor their blood pressure regularly to detect any fluctuations that may arise from dehydration. Implementing lifestyle changes, such as integrating hydrating foods into the diet and setting reminders to drink water, can support better hydration practices. Remember, if there are concerns about persistent high blood pressure or dehydration symptoms, it is important to seek medical advice promptly.
Understanding the Connection Between Fluid Loss and Hypertension

Dehydration can be an insidious enemy, silently affecting your health in ways many might not immediately recognize, including its profound impact on blood pressure. When the body is dehydrated, it experiences a reduction in blood volume, which triggers a cascade of physiological responses aimed at maintaining blood pressure. Notably, healthy fluid levels are crucial for optimal heart function and blood viscosity. Insufficient hydration can result in thickened blood, which must be pumped with greater force, leading to increased blood pressure-a critical point for anyone already managing hypertension.
The relationship between fluid loss and hypertension is amplified when we consider the body’s compensatory mechanisms. When dehydration occurs, the body activates the renin-angiotensin-aldosterone system (RAAS), a hormonal pathway intended to conserve water and maintain blood flow to vital organs. This system prompts blood vessels to constrict and releases hormones that elevate blood pressure, further complicating the health of individuals predisposed to cardiovascular problems.
To maintain control over blood pressure levels amidst the risk of dehydration, individuals should prioritize hydration by consuming adequate fluids throughout the day, particularly during exercise or in hot weather. Keep an easy rule of thumb: aim for at least eight 8-ounce glasses of water daily, and adjust based on activity levels and environmental conditions. Additionally, monitoring your blood pressure regularly can help identify fluctuations that may result from dehydration. Simple steps to stay hydrated include incorporating water-rich foods-like fruits and vegetables-into your diet. Setting reminders to drink water can also help establish a healthy routine that supports both hydration and cardiovascular health.
Remember that making small, consistent changes can lead to significant improvements in your overall health. If you notice persistent high blood pressure or symptoms associated with dehydration, such as dizziness or dry mouth, it’s vital to consult with a healthcare professional for evaluation and advice on effective management strategies. Maintaining proper hydration not only supports blood pressure regulation but also enhances overall heart health, showcasing the intricate interplay between these vital aspects of well-being.
The Physiology of Blood Pressure Regulation

When the body senses a drop in blood volume, often due to dehydration, it initiates a sophisticated set of physiological responses to maintain stable blood pressure. This process is critical because blood pressure regulation is essential for ensuring adequate blood flow to vital organs, including the heart and brain. One of the primary systems involved in this regulation is the renin-angiotensin-aldosterone system (RAAS), which is activated in response to low blood volume or blood pressure. This hormonal pathway not only conserves water but also leads to vasoconstriction-narrowing of the blood vessels-which helps increase blood pressure.
In addition to the RAAS, the body also releases antidiuretic hormone (ADH) when dehydration occurs. This hormone acts on the kidneys to reduce urine output, thus retaining more water and further influencing blood volume and pressure. This combination of hormonal responses aims to stabilize blood pressure; however, when the body is chronically dehydrated or fails to rehydrate adequately, these compensatory mechanisms can lead to elevated blood pressure as the heart must work harder to pump thicker blood.
To effectively monitor and manage blood pressure, it is essential to recognize the signs of dehydration early. Individuals can take proactive steps to ensure they remain well-hydrated, such as:
- Drinking fluids regularly: Aim for at least eight 8-ounce glasses of water daily, increasing this amount during exercise or hot weather.
- Incorporating hydrating foods: Include water-rich fruits and vegetables in your diet, such as cucumbers, tomatoes, and oranges.
- Setting reminders: Utilize phone alarms or apps to remind yourself to drink water throughout the day.
- Monitoring your body: Pay attention to symptoms of dehydration, including thirst, dry mouth, or fatigue, and take immediate action to rehydrate.
By maintaining good hydration habits, individuals not only support their blood pressure regulation but also promote overall cardiovascular health. Recognizing the interplay between hydration and blood pressure is vital in preventing potential health complications, particularly for those already managing hypertension.
Common Symptoms and Risks of Dehydration

Dehydration can be a silent but dangerous health issue that may significantly affect both your overall well-being and your blood pressure levels. Recognizing the symptoms of dehydration early is crucial for maintaining optimal health. Common signs include persistent thirst, dry mouth, and fatigue, which can easily be mistaken for other conditions, especially in busy lifestyles. More severe manifestations involve dizziness, confusion, and a noticeable decrease in urine output, often presenting as dark-colored urine. These symptoms not only affect daily functioning but can also put undue stress on cardiovascular health by forcing the heart to work harder to maintain blood pressure.
The risks associated with dehydration extend beyond temporary discomfort. Chronic dehydration may lead to elevated blood pressure as the body’s compensatory mechanisms kick in to restore volume. This process, while necessary, can inadvertently strain the heart and blood vessels, setting the stage for long-term health issues such as hypertension. Furthermore, dehydration is linked to an increased risk of kidney stones and urinary tract infections, which can contribute to further complications if not addressed promptly.
To combat these risks, maintaining hydration is essential. Consider using visual cues or scheduled reminders to encourage fluid intake throughout the day-this can help prevent the onset of dehydration symptoms. Additionally, it’s beneficial to incorporate hydrating foods, such as watermelons, cucumbers, and oranges, into your diet to support overall fluid balance. By being mindful of hydration and its impacts, individuals can take proactive steps in managing blood pressure and promoting long-term cardiovascular health.
How Dehydration Affects Heart Health

Dehydration can significantly compromise heart health, leading to a cascade of cardiovascular issues. When the body loses fluids, blood volume decreases, prompting the heart to work harder to maintain adequate circulation. This increased workload can result in higher heart rates and elevated blood pressure as the body attempts to compensate for reduced fluid levels. Over time, this chronic strain not only affects the heart muscle but also impacts the blood vessels, potentially resulting in their stiffening and narrowing, conditions associated with heart disease.
One of the primary mechanisms by which dehydration affects heart health is through the activation of stress hormones like aldosterone and vasopressin. These hormones signal the body to retain sodium and water, constricting blood vessels to conserve blood volume. While this response is essential in the short term, persistent dehydration can lead to long-term elevations in blood pressure, increasing the risk of hypertension. The interplay between low blood volume and elevated blood pressure underscores the delicate balance the body must maintain to ensure optimal heart function.
Moreover, dehydration can exacerbate other cardiovascular risk factors such as electrolyte imbalances, which are crucial for proper heart rhythm and function. An inadequate supply of electrolytes can lead to arrhythmias, or irregular heartbeats, increasing the risk of serious complications. Thus, staying hydrated is not only vital for maintaining blood pressure levels but also instrumental in supporting overall heart health.
To protect your heart, consider incorporating regular fluid intake into your daily routine. Aim for a balanced approach that includes water and hydrating foods like fruits and vegetables, while also being mindful of your activity levels and environmental conditions, which can increase fluid loss. Monitoring your hydration status and understanding the signs of dehydration-such as thirst, dry skin, or reduced urine output-will empower you to take proactive steps in safeguarding your cardiovascular health.
Evidence from Recent Studies on Blood Pressure and Dehydration
Research highlights a fascinating and intricate connection between dehydration and blood pressure, showing that fluid loss can lead to both elevated and lowered blood pressure, depending on individual circumstances. A significant study revealed that acute dehydration can immediately cause a drop in blood pressure, particularly when one moves from seated to standing positions, leading to orthostatic hypotension. In contrast, prolonged dehydration has been linked to chronic increases in blood pressure due to compensatory mechanisms in the body, such as the release of hormones that constrict blood vessels[1[1].
Moreover, clinical findings support that dehydration can trigger the secretion of hormones like aldosterone and vasopressin, which serve to conserve water and sodium. While these responses are adaptive, sustained dehydration can result in elevated blood pressure levels over time, raising the stakes for individuals at risk for hypertension. This mechanism underscores the importance of maintaining adequate hydration to avoid the dual risks of hypotension and hypertension, which can both impact cardiovascular health negatively[2[2][3[3].
By understanding these dynamics, individuals can be empowered to monitor their hydration levels actively. For instance, keeping a daily log of fluid intake and noting any symptoms of dehydration, such as increased thirst or fatigue, can be beneficial. Additionally, incorporating hydrating foods like fruits and vegetables into diets can also support optimal hydration. Recognizing the signs of dehydration and being mindful of fluid intake during hot weather or intense exercise is crucial for maintaining stable blood pressure levels and overall health.
Tips for Maintaining Optimal Hydration
Staying adequately hydrated is crucial for maintaining optimal blood pressure levels and overall health. Many people underestimate the importance of fluid intake, yet proper hydration not only supports bodily functions but also plays a significant role in regulating blood pressure. Here are some actionable tips to help you maintain optimal hydration:
- Keep a Water Bottle Handy: Having a reusable water bottle within arm’s reach can serve as a constant reminder to drink water throughout the day. Aim to consume at least eight 8-ounce glasses of water daily, adjusting for activity level and climate.
- Set Reminders: Utilize smartphone alerts or apps designed to remind you to drink water at regular intervals. This is particularly helpful for those who often forget while busy with daily tasks.
- Infuse Your Water: If plain water feels monotonous, consider infusing it with fruits, herbs, or vegetables. Combinations like cucumber and mint or lemon and berries not only enhance flavor but also add valuable nutrients.
- Monitor Urine Color: A simple way to gauge hydration is by checking the color of your urine. Pale yellow typically indicates adequate hydration, while a darker color suggests that you may need to drink more.
- Incorporate Hydrating Foods: Many fruits and vegetables have high water content and can contribute to your daily hydration goals. Watermelon, cucumbers, oranges, and strawberries are particularly effective in helping maintain fluid balance.
- Listen to Your Body: Pay attention to signs of dehydration, such as increased thirst, dry mouth, or fatigue. Addressing these signals promptly can prevent more severe hydration issues and help manage blood pressure effectively.
- Hydrate Before and After Exercise: If you’re engaging in workouts or any physical activities, ensure to drink water before, during, and after exercise to replenish lost fluids.
Incorporating these practical tips into your daily routine can empower you to stay hydrated and help manage your blood pressure effectively. Regularly monitoring your fluid intake and adjusting based on your activity levels will not only benefit your blood pressure but also enhance your overall health and well-being.
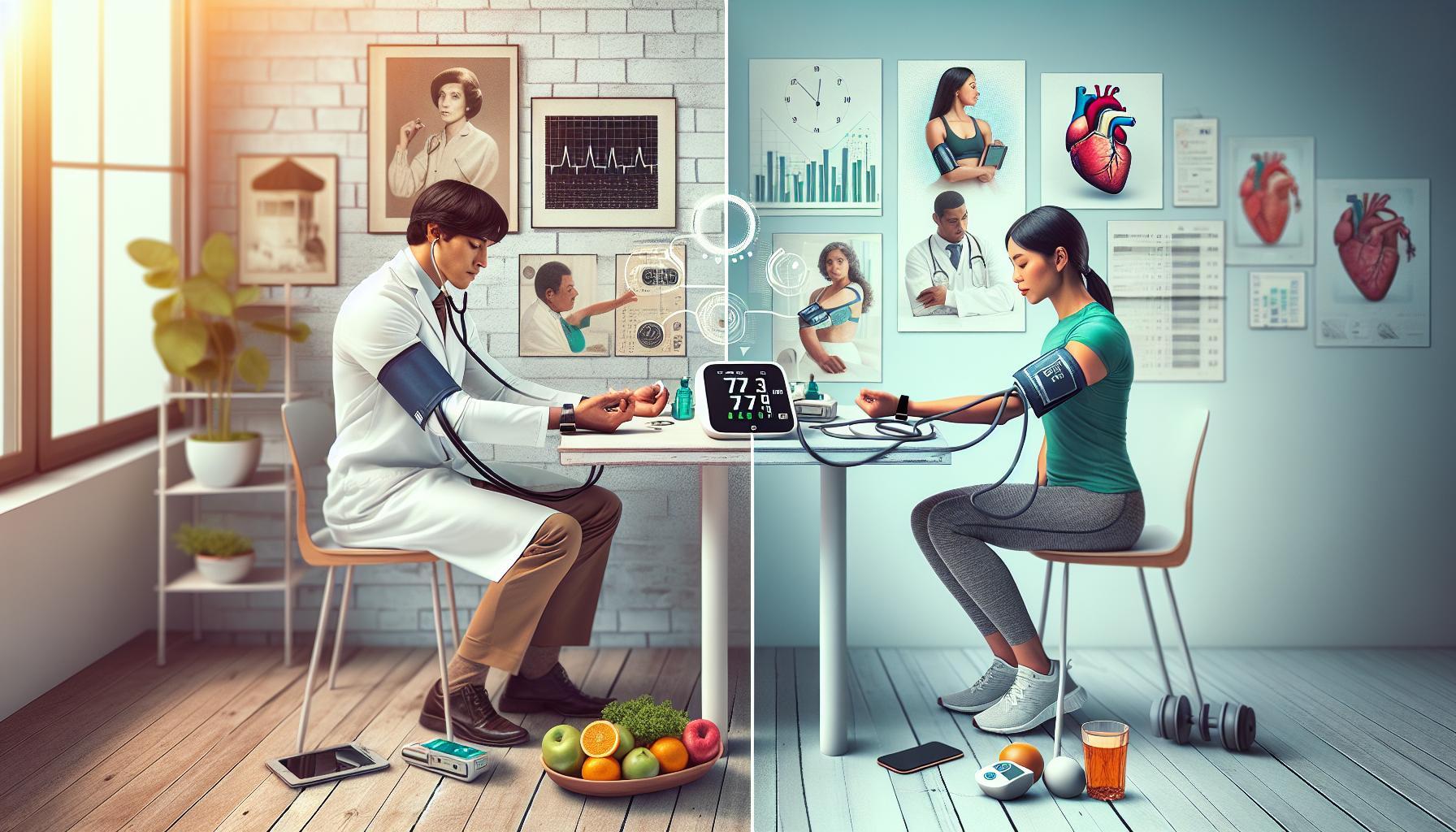
Monitoring Your Blood Pressure: What You Should Know
Monitoring blood pressure is a vital aspect of maintaining overall health, especially for those at risk of hypertension or other cardiovascular conditions. Research indicates that dehydration can lead to physiological changes that may elevate blood pressure, making it essential to stay vigilant about one’s hydration status [[2](https://mdpremier.com/the-surprising-connection-between-dehydration-and-high-blood-pressure/)]. As you embark on your journey to manage your blood pressure, understanding how to effectively monitor it can empower you to make informed decisions regarding your health.
To monitor your blood pressure accurately, consider investing in a reliable home blood pressure monitor. Regular monitoring allows you to track fluctuations and understand how different factors, including hydration levels, impact your readings. Begin by taking measurements at the same time each day for consistency, ideally after resting for at least five minutes. Note the readings and look for patterns over time. A standard guideline is to maintain a blood pressure reading below 120/80 mm Hg, and knowing your baseline will help distinguish normal variability from concerning changes.
Steps for Effective Blood Pressure Monitoring
- Choose the Right Device: Opt for a digital blood pressure monitor that provides clear readings. Ensure it is validated for accuracy.
- Position Yourself Correctly: Sit comfortably with your back supported, feet flat on the floor, and arm at heart level during measurements.
- Keep a Log: Record your readings in a journal or an app, including the time, date, and any relevant factors such as hydration status or physical activity.
- Review and Share: Discuss your readings with your healthcare provider, especially if you observe consistently high numbers or other symptoms.
By maintaining this practice, you can detect potential issues early on and make proactive lifestyle changes. If you notice significant variations tied to your hydration status-such as elevated readings after long periods without water-incorporate strategies to improve fluid intake.
Regular communication with healthcare providers is crucial, especially if you have underlying health conditions or notice concerning trends in your blood pressure. They can provide tailored advice and adjustments to your management plan based on your monitoring data. Adopting these strategies not only enhances your ability to monitor blood pressure effectively but also fosters a comprehensive approach to health management, ultimately leading to better outcomes and improved overall wellness.
Lifestyle Changes to Manage Blood Pressure Effectively
Making informed lifestyle changes can significantly impact blood pressure management, particularly in relation to hydration levels. A simple adjustment, such as ensuring proper fluid intake, can help mitigate the risks associated with dehydration and contribute to maintaining optimal blood pressure. Incorporating a few key habits into your daily routine can empower you to take control of your cardiovascular health.
An effective starting point is to prioritize hydration by setting daily water intake goals. Aim for at least 8-10 cups of water daily, adjusting based on activity levels and climate. Using a refillable water bottle can act as a visual reminder to drink consistently throughout the day. Additionally, incorporating water-rich foods like fruits and vegetables into your diet-such as cucumbers, watermelon, oranges, and spinach-can also enhance your hydration levels while providing essential nutrients that support heart health.
Regular physical activity is another crucial component of managing blood pressure. Aim for at least 150 minutes of moderate aerobic exercise each week, such as brisk walking, cycling, or swimming. Not only does exercising help regulate blood pressure, but it also enhances your hydration status through increased perspiration, making it even more critical to replenish fluids lost during workouts. Pairing your exercise routine with adequate water intake can significantly boost your overall cardiovascular health.
Furthermore, monitoring your sodium intake is vital for blood pressure management. A diet high in sodium can lead to fluid retention, which may exacerbate hypertension. Focus on consuming whole, unprocessed foods while limiting high-sodium processed snacks, fast food, and canned goods. Exploring herbs and spices as alternatives to salt can add flavor to your meals without increasing sodium levels.
In summary, by integrating these lifestyle changes-adequate hydration, regular exercise, and mindful dietary choices-you can effectively manage your blood pressure while minimizing the effects of dehydration. Small, consistent adjustments lead to significant improvements over time, allowing you to foster a healthier, more balanced life.
When to Seek Medical Advice for Blood Pressure Concerns
Regular monitoring of blood pressure is crucial, especially for those aware of the links between dehydration and hypertension. Often, individuals may overlook early warning signs, thinking they can manage their health through lifestyle changes alone. However, if you experience symptoms such as persistent headaches, dizziness, or vision changes, it’s essential to take those signals seriously. These may indicate elevated blood pressure linked to insufficient hydration or other underlying health issues.
When to Consult a Healthcare Professional
You should seek medical advice when:
- Blood Pressure Readings are Consistently High: If your readings consistently exceed 130/80 mmHg, it’s important to discuss this with a healthcare provider. Regular monitoring at home can help you track your levels accurately.
- Symptoms Persist: If you experience ongoing symptoms like fatigue, excessive thirst, or nausea, especially in conjunction with high blood pressure measurements, there could be a more serious underlying health concern.
- Significant Lifestyle Changes Fail to Help: If you’ve made considerable adjustments to your diet and hydration without seeing improvement in your blood pressure, it’s time to consult a healthcare professional for a comprehensive evaluation.
Your healthcare provider can offer tailored advice and potentially recommend diagnostic tests to assess your overall health and hydration status. In some cases, they may identify factors not previously considered, such as hormonal imbalances or kidney function issues, that may influence both hydration and blood pressure.
Engaging in open and honest discussions about your lifestyle, symptoms, and concerns enables better management strategies. Remember, timely intervention can prevent more serious complications and empower you to take control of your cardiovascular health. Prioritize your well-being and don’t hesitate to reach out for help when it’s needed.
The Role of Diet in Preventing Dehydration and Hypertension
Maintaining a balanced diet plays a crucial role in both preventing dehydration and managing hypertension. Believe it or not, everyday food choices can significantly influence your body’s hydration levels and blood pressure regulation. For instance, foods rich in water content, such as cucumbers, oranges, and tomatoes, not only provide hydration but also contribute essential nutrients that support cardiovascular health. By making informed dietary choices, you can empower yourself to maintain optimal hydration and promote healthy blood pressure levels.
A diet that includes a variety of fruits and vegetables is key to ensuring adequate fluid intake. The recommendation is to fill half your plate with colorful produce at every meal, which can improve hydration levels while delivering vital vitamins and minerals. Additionally, consider incorporating foods high in potassium, such as bananas, sweet potatoes, and spinach, as potassium helps balance sodium levels in the body, potentially lowering blood pressure. On the other hand, it’s wise to limit your intake of processed foods that are commonly high in salt, as excessive sodium can lead to fluid retention and increased blood pressure.
Hydration also goes beyond just drinking water; it’s important to consider the quality of the fluids you consume. Opt for unsweetened beverages such as herbal teas or infused waters, as sugary drinks can lead to unwanted weight gain, further complicating blood pressure management. Alcohol should also be consumed mindfully; while moderate consumption may not have adverse effects, excessive intake can lead to hydration issues and elevate blood pressure levels over time.
Ultimately, adopting a balanced diet rich in whole foods, ensuring proper hydration, and being mindful of salt intake can empower you to play an active role in your health management. Each small change matters, and by making conscious food choices, you are not only nourishing your body but also setting a solid foundation for maintaining healthy blood pressure and preventing dehydration.
Frequently Asked Questions
Q: How does dehydration affect blood pressure levels?
A: Dehydration can lead to a decrease in blood volume, resulting in lower blood pressure. However, in some cases, compensatory mechanisms may cause blood pressure to rise temporarily. It’s essential to maintain hydration for stable blood pressure control.
Q: What are the symptoms of dehydration that can impact blood pressure?
A: Symptoms of dehydration include dizziness, dry mouth, fatigue, and increased heart rate. These symptoms can indicate a drop in blood volume, potentially affecting blood pressure regulation. Monitoring hydration is vital for overall cardiovascular health.
Q: Why is hydration important for managing hypertension?
A: Proper hydration helps maintain optimal blood volume, which is crucial for regulating blood pressure. Staying hydrated can prevent fluctuations in blood pressure levels, reducing the risk of complications associated with hypertension.
Q: Can chronic dehydration lead to long-term high blood pressure?
A: Yes, chronic dehydration can contribute to hypertension by causing the body to retain sodium, increasing blood volume and pressure over time. Ensuring consistent hydration can help mitigate this risk and support heart health.
Q: How can someone improve their hydration to manage blood pressure?
A: To improve hydration, individuals should drink plenty of water throughout the day, consume hydrating foods like fruits and vegetables, and monitor fluid intake, especially during hot weather or physical activity.
Q: What role does diet play in preventing dehydration and hypertension?
A: A balanced diet rich in fruits, vegetables, and whole grains enhances hydration and provides essential nutrients that support heart health and blood pressure regulation. Foods with high water content are particularly beneficial.
Q: When should someone seek medical advice for dehydration-related blood pressure issues?
A: If symptoms of dehydration persist, accompanied by significant changes in blood pressure, medical advice should be sought. This is particularly important if there are concerns about underlying health issues influencing hydration and blood pressure.
Q: Are certain medications more likely to cause dehydration and affect blood pressure?
A: Certain antihypertensive medications, such as diuretics, can increase the risk of dehydration. It’s important to stay hydrated and consult a healthcare provider if experiencing side effects related to blood pressure medications.
For more detailed information on how dehydration and blood pressure interact, refer to sections such as “Understanding the Connection Between Fluid Loss and Hypertension” and “The Role of Diet in Preventing Dehydration and Hypertension” in the main article.
Final Thoughts
Dehydration can significantly affect your blood pressure, leading to potential health concerns that deserve your attention. Now that you understand the connection between dehydration and hypertension, it’s time to take control of your health. For ongoing support, check out our articles on effective hydration strategies and the impact of diet on blood pressure.
If you found this video helpful, we encourage you to subscribe to our channel for more insightful content, and don’t forget to comment below with any questions or experiences you’d like to share! Explore our resources further to empower yourself in managing your health daily. Remember, small changes today can lead to significant benefits tomorrow, so take the first step towards better blood pressure management.