Understanding blood pressure norms can significantly impact your health journey, especially as definitions have evolved over the decades. In 1970, normal blood pressure was generally considered to be around 120/80 mmHg. Today, however, guidelines reflect a deeper understanding of cardiovascular health, with numbers as low as 130/80 mmHg being deemed normal for many adults.
This shift is not just a matter of numbers; it speaks to the growing awareness of hypertension risks and the importance of proactive health management. With rising rates of high blood pressure, knowing how these standards have changed can empower you to make informed decisions about your health. As we explore the contrast between past and present, you’ll uncover valuable insights into why monitoring your blood pressure is crucial and how even slight changes can affect your overall well-being. Join us to learn more about these important developments and how they relate to your lifestyle today.
What Was Considered Normal Blood Pressure in 1970?
In 1970, blood pressure norms were notably different from today’s standards, reflecting both evolving medical research and a changing understanding of cardiovascular health. During that era, a blood pressure reading of 140/90 mmHg was often regarded as normal for adults. This threshold for hypertension has since shifted lower, with current guidelines classifying readings at or above 130/80 mmHg as hypertensive. This change underscores the medical community’s growing awareness of the risks associated with elevated blood pressure and the importance of early intervention.
Understanding these historical norms is crucial as they provide context for how blood pressure management strategies have developed over time. The 1970s marked an era where there was less emphasis on routine monitoring and preventive care. Many individuals were unaware of the silent risks associated with high blood pressure, often referred to as the “silent killer” due to its lack of obvious symptoms. Consequently, individuals frequently faced serious health consequences, including heart disease and stroke, without recognizing their hypertensive status.
The shift in perception around what constitutes healthy blood pressure is a reflection of broader changes in healthcare practices and lifestyle awareness. Increased access to blood pressure monitoring tools and educational resources has empowered people to take charge of their health. Today, regular blood pressure checks are encouraged, and lifestyle modifications such as improved diet, increased physical activity, and stress management are recognized as critical components for maintaining healthy blood pressure levels. By understanding the past, individuals can better appreciate their current health status and the ongoing importance of proactive health management.
Changes in Blood Pressure Guidelines Over the Decades
The evolution of blood pressure guidelines over the decades reflects a significant shift in our understanding of cardiovascular health and the importance of early intervention. In the 1970s, a blood pressure reading of 140/90 mmHg was commonly accepted as the threshold for hypertension. This standard was largely based on outdated epidemiological data and clinical practices, with fewer studies focusing on the detrimental effects of even slightly elevated readings. However, as research advanced and the link between hypertension and severe health outcomes became clearer, the medical community began to reassess these standards.
By the 2000s, new guidelines recommended a lower threshold for hypertension, officially marking the cutoff at 130/80 mmHg. This shift was influenced by accumulating evidence demonstrating that even mildly elevated blood pressure could significantly increase the risk of cardiovascular diseases, stroke, and renal failure. Organizations such as the American College of Cardiology and the American Heart Association took a proactive stance, emphasizing the necessity for earlier detection and treatment, thereby reshaping the landscape of hypertension management.
As guidelines have evolved, so too have strategies for monitoring blood pressure. With advancements in technology, home blood pressure monitors have become more accessible, empowering individuals to track their health proactively. This shift promotes a greater understanding of one’s blood pressure readings, leading to informed lifestyle choices. Regular monitoring not only allows for timely medical intervention but also encourages healthier behaviors, such as diet changes and increased physical activity, which are recognized as essential in managing blood pressure levels.
Moreover, the conversation surrounding blood pressure management has expanded to include not just medication but also comprehensive lifestyle modifications. Diet, exercise, and stress management have gained recognition as cornerstones of effective blood pressure control. Healthcare providers increasingly advocate for a holistic approach, empowering patients with the knowledge and tools necessary to maintain healthy blood pressure levels over time. This transition from a reactive to a proactive approach in managing hypertension exemplifies a dynamic shift in public health ethos, significantly reducing the risks associated with high blood pressure for future generations.
Factors Influencing Blood Pressure Norms: A Historical Perspective
In the 1970s, blood pressure norms were shaped by a combination of prevailing medical beliefs, technological limitations, and the socio-economic context of the time. A blood pressure reading of 140/90 mmHg was widely considered the threshold for hypertension. This perspective stemmed from earlier studies that mainly focused on severe cases of high blood pressure and their obvious consequences. Consequently, only the most elevated readings were deemed concerning, largely overlooking the incremental risks posed by lower levels of hypertension.
Over the decades, various factors have prompted a reevaluation of what constitutes “normal” blood pressure. Advancements in medical research have highlighted the relationship between slightly elevated blood pressure and various adverse health outcomes, such as heart attacks and strokes. As more data became available, particularly through longitudinal studies and population health data, health professionals began to recognize that levels lower than previously thought could also contribute to significant health risks.
Technological Advances and Public Awareness
The rise of more sophisticated blood pressure monitoring technologies also played a critical role in changing perceptions. During the 1970s, measurement tools were often less accessible to the general public. However, with the advent of user-friendly digital monitors and increasing health consciousness, people began to take a more proactive stance on their health. This empowerment led to greater awareness of blood pressure management among the general populace.
Moreover, societal changes, such as the increasing prevalence of sedentary lifestyles and poor dietary habits, prompted public health campaigns to focus on preventive measures. These campaigns have been instrumental in reshaping perceptions of blood pressure norms, pushing towards lower thresholds for hypertension to mitigate the rising rates of cardiovascular diseases in the population.
Conclusion
Understanding the historical context of blood pressure norms provides valuable insights into why current guidelines emphasize earlier intervention and lower thresholds for hypertension. Recognizing that optimal blood pressure management hinges on both accurate measurement and a proactive approach to health can encourage individuals to engage more effectively in their own health management strategies. Armed with knowledge and tools, people can make informed lifestyle changes that support long-term cardiovascular health, transforming prior norms into a vision of prevention and wellness.
How Lifestyle Changes Impact Blood Pressure Readings
Making simple lifestyle adjustments can significantly influence blood pressure readings, transforming overall health and well-being. Just as societal norms surrounding blood pressure have evolved from the 1970s to today, so too have our understanding and management of the factors that affect these readings. Consider that recent studies indicate a staggering 1 in 3 adults in the U.S. experience high blood pressure-an issue that can often be mitigated with informed lifestyle choices.
One of the most impactful ways to manage blood pressure is through diet. A balanced diet high in fruits, vegetables, whole grains, and lean proteins can play a pivotal role in maintaining healthy blood pressure levels. Foods rich in potassium, such as bananas and spinach, can help lower blood pressure by counteracting sodium’s effects. Conversely, a diet high in processed foods, sugars, and saturated fats can lead to elevated blood pressure. Emphasizing whole, nutrient-dense foods can help individuals attune their diets to better control their blood pressure.
Regular physical activity is another cornerstone of blood pressure management. Engaging in at least 150 minutes of moderate aerobic exercise each week, such as brisk walking or cycling, can lower systolic and diastolic blood pressure significantly. Exercise strengthens the heart, allowing it to pump blood more efficiently and reducing pressure on artery walls. Moreover, integrating activities like yoga or tai chi can also help alleviate stress, contributing to overall blood pressure reduction.
Stress management strategies, such as mindfulness, meditation, and adequate sleep, contribute equally to blood pressure control. Chronic stress has been linked to increased hypertension, making it essential for individuals to find coping mechanisms that work for them. Whether through breathing exercises or engaging hobbies, prioritizing mental well-being can yield tangible benefits, improving blood pressure readings.
To effectively monitor changes, it’s advisable to track blood pressure regularly using a home monitor. Keeping a log of readings can provide both patients and healthcare providers with valuable insights, helping to tailor individualized management plans. By adopting these lifestyle changes, individuals can empower themselves to take control of their health and potentially reduce their risk of cardiovascular disease.
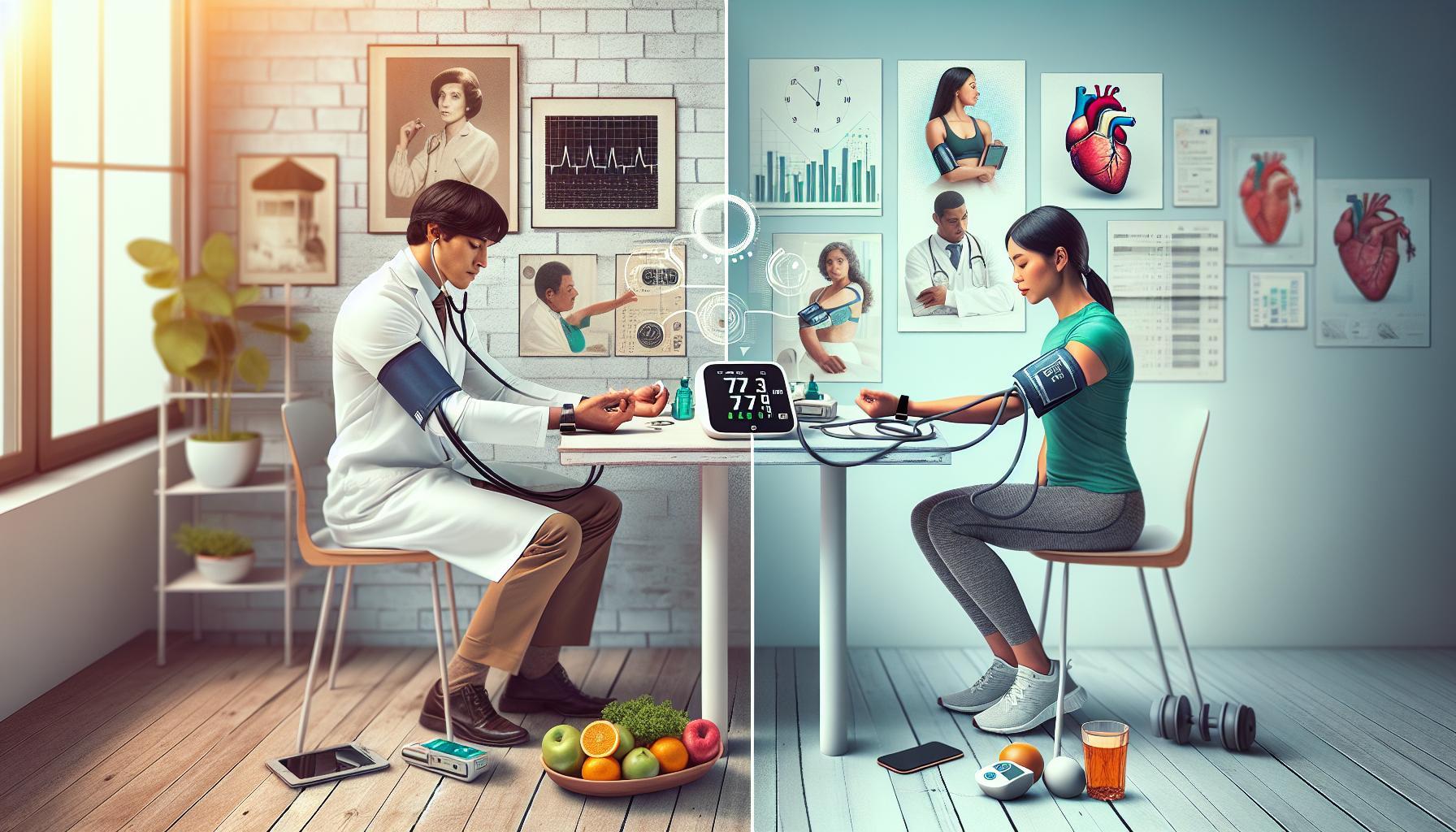
Comparing Blood Pressure Measurement Techniques: Then and Now
Blood pressure measurement techniques have evolved significantly from the 1970s to today, reflecting advancements in technology and a deeper understanding of cardiovascular health. In the past, healthcare professionals predominantly relied on mercury sphygmomanometers-devices that used a column of mercury to gauge blood pressure. This method, while effective, had drawbacks such as difficulties in transport, risk of mercury exposure, and the requirement for manual reading, which could lead to human error. Today, digital monitors that provide automated readings have become commonplace, allowing for more accurate and user-friendly blood pressure assessments.
The methodologies for measuring blood pressure have also changed. Previously, readings were taken in a somewhat noisy clinical environment, potentially causing anxiety that could skew results. Modern guidelines recommend a more controlled setting: individuals should be seated comfortably, avoid vigorous activity beforehand, and remain quiet during the measurement to ensure accuracy. Additionally, it’s now advised to take multiple readings over a span of days to obtain a more accurate depiction of an individual’s blood pressure.
At-Home Monitoring
An equally significant shift is the emphasis on at-home monitoring. Patients are encouraged to measure their blood pressure regularly using personal monitors, fostering greater awareness and engagement in their health management. These devices have drastically improved with intuitive designs and Bluetooth technology that syncs data to mobile apps, making it easier to track changes and share information with healthcare providers.
When measuring blood pressure at home, consider the following steps:
- Ensure the monitor is validated and fits properly on your arm.
- Take readings at the same time each day, ideally in the morning and evening.
- Follow the manufacturer’s instructions for use, ensuring a quiet environment to minimize distractions.
It’s important to note that not all devices are created equal. Choose between automatic or manual machines, and invest in one that best suits your comfort and needs.
Understanding the Readings
Whether using traditional or modern techniques, understanding the numbers remains crucial. Blood pressure readings are given as two numbers: the systolic pressure (the force of blood against the artery walls during a heartbeat) over diastolic pressure (the force of blood in the arteries when the heart rests between beats). Recognizing what constitutes high or low readings aids in timely intervention and lifestyle adjustments.
With these advancements, individuals now have the tools to take proactive steps in understanding and managing their blood pressure, helping to mitigate the risks associated with hypertension effectively. Embracing these modern techniques empowers individuals to maintain better health and make informed decisions in their journey toward cardiovascular wellness.
Understanding Blood Pressure: What Do the Numbers Mean?
Understanding blood pressure readings is essential for managing cardiovascular health effectively. Blood pressure is measured in millimeters of mercury (mmHg) and consists of two numbers: systolic and diastolic. The systolic pressure, represented by the upper number, indicates the force of blood against artery walls when the heart beats, while the diastolic pressure, represented by the lower number, reflects the pressure in the arteries between heartbeats when the heart is resting.
A common question is: what do these numbers mean in practical terms? Blood pressure categories help contextualize these readings. Normal blood pressure is generally considered to be around 120/80 mmHg. Readings above this can indicate various health issues. For instance, systolic readings between 120-129 mmHg are classified as elevated blood pressure, while 130 mmHg or higher is considered high blood pressure or hypertension. Understanding these thresholds can empower individuals to recognize the need for lifestyle changes or seek medical attention.
In the context of historical norms from the 1970s, it’s important to note that what was once considered acceptable has evolved. Decades ago, slightly higher readings might have been overlooked, but modern guidelines emphasize earlier intervention for readings that exceed 130/80 mmHg. This shift reflects a deeper understanding of the risks associated with hypertension, including heart disease and stroke.
Monitoring your blood pressure at home provides valuable insights into your health. Here are some practical steps to accurately gauge your blood pressure:
- Choose the right time: Measure your blood pressure at the same times each day, ideally in the morning and evening.
- Stay relaxed: Sit quietly for a few minutes before taking the reading to minimize any nervousness that could skew results.
- Use the same arm: Consistency in the arm you use for measurements can lead to more reliable tracking.
- Record your readings: Keeping a log of your blood pressure over time can help identify trends or when to consult a healthcare provider.
By developing an understanding of what your blood pressure readings signify, you can take informed steps towards better heart health, whether that means focusing on diet and exercise or discussing medication with your doctor.
The Role of Diet and Exercise in Blood Pressure Management
Lifestyle choices, particularly diet and exercise, play a crucial role in managing blood pressure effectively. Nearly half of American adults live with high blood pressure, making it imperative to adopt evidence-based strategies that can lower these numbers. Interestingly, studies have shown that even modest lifestyle changes can significantly influence blood pressure readings, leading to improvements over time.
A well-balanced diet is foundational in blood pressure management. The American Heart Association emphasizes the benefits of the DASH (Dietary Approaches to Stop Hypertension) diet, which prioritizes fruits, vegetables, whole grains, and lean proteins while reducing saturated fat, cholesterol, and sodium. Specifically, limiting sodium intake to less than 2,300 mg per day (ideal target being 1,500 mg) can lead to a reduction in systolic blood pressure by approximately 5 to 6 mmHg. Foods rich in potassium, such as bananas, sweet potatoes, and spinach, can counteract the effects of sodium and are beneficial for maintaining healthy blood pressure levels.
Exercise is equally vital. Regular physical activity strengthens the heart, enabling it to pump blood more efficiently and reducing the strain on arteries. The American Heart Association recommends at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week. Activities like brisk walking, cycling, and swimming can lead to a reduction in blood pressure of about 4 to 9 mmHg. Incorporating strength training at least twice a week can also enhance these benefits by improving overall cardiovascular health.
To effectively manage blood pressure through lifestyle changes, consider these actionable steps:
- Plan meals: Create weekly meal plans focusing on DASH-friendly foods to foster healthier eating habits.
- Set exercise goals: Aim for daily activity; start with 10-minute increments and gradually increase duration.
- Monitor your progress: Keep a journal of dietary choices and exercise routines, as tracking can motivate and reflect progress.
- Stay hydrated: Drinking sufficient water can help maintain kidney function, which is essential for blood pressure control.
By understanding the profound impact that diet and exercise can have on blood pressure, individuals can take empowered steps towards enhancing their cardiovascular health, aligning with modern guidelines and shifting perceptions of what constitutes healthy blood pressure management.
Common Myths About Blood Pressure: Debunked
Many misconceptions surround blood pressure, which can lead to mismanagement and increased health risks. One prevalent myth is that high blood pressure only affects older adults. In reality, hypertension can affect individuals of all ages, including young and middle-aged people. This misconception often leads to a lack of awareness and monitoring among younger adults, putting them at risk for long-term health consequences.
Another common belief is that having “white coat syndrome”-elevated blood pressure readings due to anxiety during doctor’s visits-means that one does not have to worry about high blood pressure. While it’s true that anxiety during a medical examination can temporarily raise blood pressure, this does not negate the importance of monitoring blood pressure regularly. Individuals should seek to check their blood pressure outside of these settings, as consistent high readings, regardless of context, indicate the need for further evaluation and possible intervention.
A third myth is the notion that high blood pressure isn’t dangerous if there are no noticeable symptoms. This is particularly dangerous, as hypertension is often called the “silent killer” because many individuals do not experience symptoms until serious damage has been done to their cardiovascular system. Regular monitoring is crucial, as early detection can lead to effective management and prevention of complications such as heart disease and stroke.
Lastly, some people believe that simply taking medication for high blood pressure will suffice without making lifestyle changes. While medication is essential for many individuals, lifestyle modifications-such as improved diet, increased physical activity, and stress management-play a significant role in overall blood pressure health. Embracing these changes can enhance the effectiveness of medications and lead to better health outcomes.
Understanding and debunking these myths empowers individuals to take control of their blood pressure health. Regular monitoring, awareness of both inner and outer health trends, and proactive lifestyle choices are essential steps toward maintaining optimal blood pressure and overall well-being.
The Importance of Regular Blood Pressure Monitoring
Monitoring blood pressure regularly is crucial in the battle against hypertension and maintaining overall health, as early detection can significantly alter the trajectory of cardiovascular issues. A staggering fact is that nearly half of the adults in the United States have high blood pressure, often without experiencing any symptoms. This “silent” nature of hypertension underscores the importance of routine monitoring; what’s considered normal today may have shifted compared to standards from the 1970s.
To effectively monitor blood pressure, individuals should follow a structured approach:
- Frequency: For those with normal readings, checking blood pressure at least once a year is advisable. However, individuals with elevated readings or risk factors should monitor their levels more frequently, ideally at home and during doctor visits.
- Technique: Use a validated blood pressure monitor and ensure it fits properly. Sit in a relaxed position with your back supported and feet flat on the floor for at least five minutes before taking a reading. Measure at the same time of day to maintain consistency.
- Record Keeping: Keep a log of your readings, noting the date, time, and any relevant activities prior to measurement. This can help healthcare providers understand your blood pressure trends and make informed recommendations.
With the efficacy of lifestyle changes becoming increasingly acknowledged, regular monitoring aids in assessing the impact of diet, exercise, and stress management on blood pressure. For instance, after implementing a low-sodium diet or a new exercise routine, monitoring your blood pressure regularly can reveal positive trends, motivating further adherence to these healthy behaviors.
Moreover, understanding the implications of your readings is vital. The American Heart Association defines normal blood pressure as below 120/80 mm Hg. Anything above this threshold can signal elevated concerns, which may have been perceived differently in the past. For context, in the 1970s, the acceptable range was often considered higher, reflecting a broader acceptance of elevated readings. Awareness of these changing standards can empower individuals to take charge of their health, reinforcing the idea that proactive measures today can mitigate the risks associated with hypertension in the future.
In conclusion, the significance of regular blood pressure monitoring cannot be understated; it serves as a key indicator of cardiovascular health, encourages lifestyle changes, and fosters an active partnership in personal health management. Embracing this practice not only shields against potential complications but also cultivates a deeper understanding of one’s health and wellbeing.
Health Risks of High Blood Pressure: Past and Present
The implications of high blood pressure, often termed hypertension, have undergone significant evolution over the decades, impacting how individuals understand and manage their health. In the past, particularly in the 1970s, the thresholds for what was considered “normal” were notably higher, leading to a greater acceptance of elevated blood pressure readings. This leniency contributed to an era when the health risks associated with hypertension were often underestimated, ultimately resulting in a surge of cardiovascular-related health issues that defined the landscape of public health.
Today, the stark reality of high blood pressure is more pronounced, with emerging research continually linking hypertension to severe health complications, including heart disease, stroke, and kidney failure. Increased awareness has highlighted that even slightly elevated blood pressure can precipitate a cascade of health problems. The current medical consensus maintains that a reading above 120/80 mm Hg is cause for concern, suggesting that preventive measures should be taken well before blood pressure becomes critically high. This proactive approach starkly contrasts with the attitudes of previous decades, making early intervention and lifestyle modifications essential.
Understanding the health risks associated with high blood pressure can empower individuals to take control of their health through informed choices. These risks remain consistent, yet the emphasis on prevention has intensified. For instance, uncontrolled hypertension can lead to the thickening of the heart’s walls, making it harder for the heart to pump blood, potentially leading to heart failure and other serious complications. Regular monitoring, lifestyle adjustments, and medication adherence, when necessary, remain pivotal in mitigating these risks.
To effectively combat high blood pressure, consider integrating these practical strategies into your daily routine:
- Dietary Adjustments: Embrace a heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, which emphasizes fruits, vegetables, whole grains, and lean proteins while reducing sodium intake.
- Regular Physical Activity: Aim for at least 150 minutes of moderate exercise weekly, which can lower blood pressure and strengthen your heart.
- Stress Management: Engage in stress-reduction techniques such as yoga, meditation, or deep-breathing exercises to support overall heart health.
- Consistent Monitoring: Make monitoring your blood pressure a regular part of your healthcare routine, recording your readings and sharing them with your healthcare provider to track your progress.
Navigating the landscape of blood pressure health is vital for longevity and quality of life. By understanding the past and recognizing the present risks, individuals can forge a path toward better health management, equipped with the knowledge to make impactful lifestyle changes today.
Future Trends in Blood Pressure Management and Guidelines
The landscape of blood pressure management is continuously evolving, driven by a confluence of innovative research, technological advancements, and a growing emphasis on preventive health. One of the most promising trends is the integration of digital health technologies, such as smartphone apps and wearable devices, which empower individuals to monitor their blood pressure with ease and accuracy. These tools not only offer convenience but also facilitate real-time data collection that can be shared with healthcare providers, allowing for more personalized treatment plans and timely interventions.
As guidelines tighten and the importance of early detection rises, healthcare professionals are increasingly advocating for routine blood pressure screenings, even in younger populations. This shift underscores the notion that hypertension does not discriminate by age, and acknowledging this can lead to significant improvements in long-term health outcomes. Educational campaigns and public health initiatives aim to inform communities about the risks of hypertension and the importance of proactive monitoring. By normalizing conversations around blood pressure, we can dismantle the stigma and complacency that may have existed in past decades, particularly when considering the higher thresholds accepted in the 1970s.
Investments in research are also leaning toward understanding the genetic and environmental factors that contribute to hypertension, leading to more tailored treatments. Discoveries in pharmacogenomics, for example, are enabling doctors to prescribe medications that are more effective based on an individual’s genetic profile, enhancing efficacy while reducing the likelihood of side effects. This personalized approach not only increases patient adherence but also invites a new era of tailored lifestyle advice that complements medical treatment.
To optimize blood pressure management, consider the following actionable strategies:
- Embrace Technology: Utilize blood pressure monitoring apps and devices that sync with your smartphone to keep track of your readings and share them with your doctor.
- Take Preventive Action: Schedule regular check-ups, and discuss your blood pressure history with your healthcare provider to help guide your monitoring schedule.
- Invest in Education: Participate in community health programs focused on hypertension awareness, which can provide valuable resources and support networks.
- Adopt a Holistic Approach: Engage in discussions about diet, exercise, and stress management techniques with your healthcare providers to create a comprehensive health plan.
As we look to the future, it is clear that we are moving towards a more proactive, informed, and personalized approach to blood pressure management. This paradigm shift not only fosters greater awareness but also equips individuals with the necessary tools to maintain their health, ultimately leading to a reduction in hypertension-related complications.
Empowering Your Health: Steps to Maintain Healthy Blood Pressure
Maintaining healthy blood pressure is not just about monitoring numbers; it’s about adopting a lifestyle that supports your overall well-being. With blood pressure being a key indicator of heart health, understanding and managing this vital parameter empower individuals to take charge of their health journeys. Research indicates that hypertension is a silent adversary, often going unnoticed until serious complications arise. Therefore, proactive measures to maintain optimal blood pressure are crucial.
To effectively manage your blood pressure, consider implementing the following actionable strategies:
- Regular Monitoring: Make blood pressure checks a routine part of your healthcare regimen. Utilize home monitoring devices to track readings, ensuring you understand your baseline. This vigilance allows for timely adjustments and discussions with your healthcare provider.
- Healthy Diet: Embrace a heart-healthy eating plan, such as the DASH (Dietary Approaches to Stop Hypertension) diet. Focus on consuming fruits, vegetables, whole grains, and lean proteins while limiting processed foods high in salt and sugar.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise weekly. Activities like walking, cycling, or swimming not only help lower blood pressure but also enhance overall cardiovascular health.
- Weight Management: Maintaining a healthy body weight can significantly lower your risk of developing hypertension. Monitor your weight regularly and adopt healthy eating and physical activity habits to achieve and sustain your ideal weight.
- Stress Reduction: High stress can impact blood pressure. Incorporate stress management techniques such as yoga, meditation, or deep-breathing exercises to cultivate relaxation and emotional resilience.
Incorporating these practices can fundamentally shift how you manage your health. It’s essential to recognize that everyone’s body responds differently. Therefore, consulting with a healthcare professional for personalized advice and guidance ensures that your strategies align with your unique health profile.
Furthermore, understanding what blood pressure numbers mean is critical. Generally, a reading of less than 120/80 mmHg is considered normal, whereas numbers in the ranges of 120-129 systolic and less than 80 mmHg diastolic indicate elevated pressure. Consistently high readings may require intervention, hence why regular monitoring is imperative.
By embracing these steps and actively participating in your health management, you not only foster a proactive attitude towards blood pressure control but also enhance your overall quality of life. Whether you are navigating potential hypertension or seeking to maintain a healthy range, every small action contributes to significant outcomes in your health journey. Empower yourself with knowledge and resources, and take confident strides toward a healthier future.
Frequently Asked Questions
Q: What was the average normal blood pressure in the 1970s?
A: The average normal blood pressure in the 1970s was typically considered to be around 120/80 mmHg. However, many health experts acknowledged higher readings as acceptable based on individual health conditions and demographic factors of the time.
Q: How have blood pressure measurement methods changed since the 1970s?
A: Blood pressure measurement methods have evolved significantly since the 1970s, transitioning from manual sphygmomanometers to digital monitors. This advancement has improved accuracy and ease of use, enabling more consistent monitoring and detection of hypertension.
Q: Why have blood pressure guidelines changed over the years?
A: Blood pressure guidelines have changed due to increased understanding of cardiovascular health and risk factors. Research into the effects of high blood pressure on health outcomes has led to more stringent guidelines aimed at reducing the incidence of heart disease and stroke.
Q: What lifestyle changes contribute most to keeping blood pressure normal today?
A: Lifestyle changes that help maintain normal blood pressure include adopting a balanced diet rich in fruits and vegetables, engaging in regular physical activity, reducing salt intake, and managing stress. These practices are crucial to preventing hypertension.
Q: How does high blood pressure today compare to that of the past?
A: High blood pressure rates today are often attributed to lifestyle and dietary changes, marking a significant increase compared to the past. Many people today are diagnosed with hypertension earlier, emphasizing the importance of regular monitoring and prevention strategies.
Q: What are common myths about blood pressure that have persisted since the 1970s?
A: Common myths about blood pressure include the belief that only elderly people experience hypertension and that it is unrelated to diet. Both myths overlook the fact that hypertension can affect individuals of all ages and that diet plays a vital role in blood pressure management.
Q: How can individuals monitor their blood pressure effectively at home?
A: Individuals can monitor their blood pressure at home by using a validated digital monitor, ensuring proper technique-like sitting quietly for at least five minutes before taking the reading. Regularly tracking measurements can help identify trends and manage health effectively.
Q: What factors influenced blood pressure norms in the 1970s versus now?
A: Factors influencing blood pressure norms include dietary habits, physical activity levels, stress, and the prevalence of obesity. In the 1970s, there was less prevalence of processed foods and sedentary lifestyles compared to today, which have contributed to rising hypertension rates.
To Wrap It Up
As we’ve explored, understanding the evolution of what constitutes normal blood pressure from 1970 to today is crucial for your health management. With rising health awareness, it’s essential to monitor your blood pressure regularly and adopt lifestyle changes that promote cardiovascular wellness. Are you ready to take control? Consider checking out our guide on effective monitoring techniques and diet tips to support healthy blood pressure levels.
Don’t hesitate to dive deeper into related topics such as common misconceptions about hypertension or the latest guidelines on blood pressure management. For continuous updates and personalized insights, subscribe to our newsletter today! Your journey towards better health starts now-share your thoughts below or join our community for support and motivation. Together, we can navigate your health journey effectively!